Reproduced from Shutterstock Via Subscription
I am often asked to consult on managing patients with elevated lipid levels. Some of these patients have had their lipid measured monthly by their clinicians for years. That seems like a waste of time, money, and blood. So, what lipids should you measure and how often should you repeat them?
Baseline lipid measurement requires a lipid panel including total cholesterol (TC), HDL-C, triglycerides (TGs), and LDL-C. I routinely measure thyroid stimulating hormone (TSH) because of the rule, “Any patient with a lipid disorder is hypothyroid until you prove it otherwise.” (1) That’s because you need thyroid hormone to make LDL receptors so hypothyroidism can increase LDL levels. Thyroid hormone also increases lipoprotein lipase (LPL) activity, and LPL decreases TGs and increases HDL-C, so high TGs and a low HDL-C can be due to hypothyroidism. Hypothyroidism also increase lipoprotein (a).
I also measure hemoglobin A1C if the TGs are increased. That’s because of the
rule that “every patient with hypertriglyceridemia is a ‘diabetic-want-to-be’ until proven otherwise. (2) It takes more insulin to regulate TG metabolism than it does to regulate glucose metabolism, so elevated TGs are an early sign of insulin resistance whereas elevated glucose levels are a late sign. Many patients with insulin resistance present with high TGs years before their A1C bumps. If they have high TGs and a borderline A1C (around 5.7%), I do a 2-hour oral glucose tolerance test to detect early insulin resistance.
I also like to get a lipoprotein (a) level [Lp(a)] because Lp(a) is such an important, underappreciated marker of risk. Lp(a) makes any lipid profile more dangerous. I measure Lp(a) to avoid giving “false reassurance”. (3) Some insurance companies will not cover the cost of the Lp(a) measurement, so warn the patient that they may get charged about $30 for the test.
I also like to get an apolipoprotein B level (apo B). Apo B is a better measure of atherosclerotic risk than LDL-C. LDL particles vary in their cholesterol content, with small dense particles being most atherogenic. But every atherogenic particle contains only one apo B so an apo B level tells you how many atherogenic particles there are. Atherosclerosis is a chemical reaction in the endothelium, and all chemical reactions accelerate with more molecules to act as reagents. Think of the Apo B-containing particles as if they were reagent molecules. Apo B tells you how many reagent particles there are floating around and capable of entering the endothelium to accelerate the reaction. The Apo B treatment goal is 10 points higher than the LDL-C treatment goal.
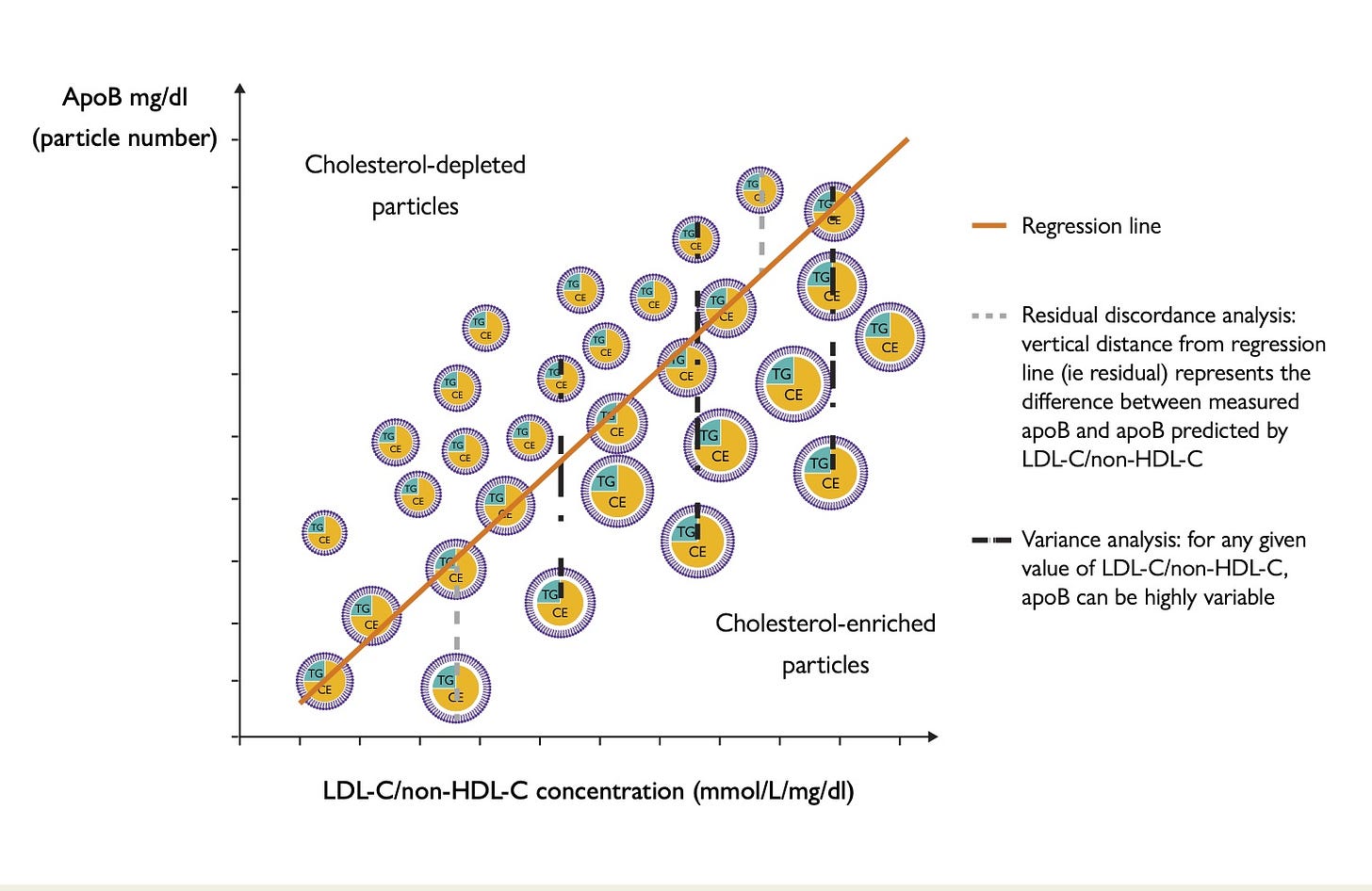
Some lipid experts think that an apo B level is not needed because non-HDL-C is a good surrogate for the apo B level. Non-HDL-C is calculated by subtracting HDL from the total C. This measurement correlates tightly with apo B in populations, but poorly in individual patients. So, the correlation line of non-HDL-C vs apo B is very linear, but the dots for the individual patients are all over the place. Dr. Alan Sniderman, an expert in apo B at McGill, has said, “Do you take care of lines (populations) or dots (individuals)”? I have included a figure from one of Dr. Sniderman’s papers. (4)
Reproduced from (4) for educational purposes only.
It shows that the cholesterol content of LDL particles vary, and that the apo B level correlates well in the population with the ratio of LDL-/non-HDL-C, but not well for individual subjects. This is not exactly apo B versus non-HDL-C, but it is the same principle.
When should lipid levels be repeated?
I generally repeat lipid levels yearly in someone on a stable medical regimen. Medicare may not cover more than one measurement per calendar year unless there has been a medication change.
I generally do not repeat Lp(a) measurements. Lp(a) is primarily genetically determined, so most authorities suggest a “one and done” measurement. I generally agree, but repeating the measurement can be justified:
· After starting a proprotein convertase subtilisin/kexin type 9 inhibitor (PCSK9i) because they reduce Lp(a) about 20%.
· After puberty if it was elevated before puberty because both estrogen and androgens lower Lp(a). We demonstrated the testosterone effect almost 25 years ago. (5)
· After menopause because estrogen reduces Lp(a) so menopause increases it.(6)
I repeat the lipid levels about 3 weeks after starting someone on a statin, ezetimibe or bempedoic acid. The effect of these drugs is near-maximal after just 2 weeks, but I usually wait 3-4 weeks. I don’t wait longer because I want the patient to get prompt, positive reinforcement that the drugs work. That should help with compliance. I then repeat the measurement every 12 months.
The PCSK9i manufacturers recommend repeating measurements 6 to 8 weeks after starting the drug. I usually do it at 6 weeks, but I always measure 1-3 days before the next injection even with inclisiran which only needs to be given every 6 months. I do this because the PCSK9i lipid-lowering effect dissipates with time in some patients, at least with the every-two-week agents, and I want to see what is the minimal effect of the drug so I can increase the dose if necessary. (7)
The effects of fenofibrate and other fibric acid derivatives and concentrated fish oil (all of which I still use for managing TGs over 500 mg/dl ) are also quite prompt, so the TGs can be measured 3-4 weeks after starting these drugs. The effect of niacin on TGs and LDL-C is also prompt, but the effect on HDL-C evolves over a prolonged period of time, such as 12 months. I bring that up because it’s interesting, and not widely known, but almost nobody still uses niacin. I still do use it occasionally for both LDL-C and Lp(a).
So, the rules for What Lipids Should You Measure, When And How Often are:
· Measure lipids, A1C, TSH at baseline
· Measure Lp(a) to avoid giving false reassurance.
· Measure apo B to know particle number. You don’t really need the fancy “advanced lipid testing” tests.
· Remember that every patient with elevated TGs may be a diabetic-want-to-be.
· Repeat lipid measurements 3-4 weeks after changing meds or yearly if they are on a stable medical regimen.
· Measure PCSK9i’s effects several days before the next injection – the likely time of least lipid reduction.
References
1. https://pauldthompsonmd.substack.com/p/every-patient-with-any-lipid-disorder. Accessed July 26, 2024.
2. https://pauldthompsonmd.substack.com/p/diabetic-want-2-bs. Accessed July 26, 2024.
3. https://pauldthompsonmd.substack.com/p/dont-give-false-reassurance. Accessed July 26, 2024.
4. Allan D Sniderman, Line Dufresne, Karol M Pencina, Selin Bilgic, George Thanassoulis, and Michael J Pencina .Discordance among apoB, non–high-density lipoprotein cholesterol, and triglycerides: implications for cardiovascular prevention. Eur Heart J. 2024 Jul 14; 45(27): 2410–2418. PMID: 38700053
5. Nouf Aljawini, Lateefa O. Aldakhil, Syed Shahid Habib. High-Risk Lipoprotein(a) Levels in Saudi Women and Its Relationship to Menopause and Adiposity. Nutrients. 2023 Feb; 15(3): 693. PMC9919220
6. Zmunda JM, Thompson PD, Dickenson R, Bausserman LL. Testosterone decreases lipoprotein(a) in men. Am J Cardiol. 1996 Jun 1;77(14):1244-7. PMID: 8651107
7. Elfar A, Thompson PD.Variability in low density lipoprotein-cholesterol concentrations after alirocumab injection. .J Clin Lipidol. 2017 Jan-Feb;11(1):307. PMID: 28391904
#lipid #lipidmeasurement #cholesterol #triglycerides #apoliprotein B #lipoprotein(a) #diabetes #hypothyroidism #estrogen #androgen #testosterone #thyroid



Thank you. Paul
Excellent article