Diabetic Want 2 B’s
A Patient with Hypertriglyceridemia is a Diabetic or Pre-Diabetic Until Proven Otherwise
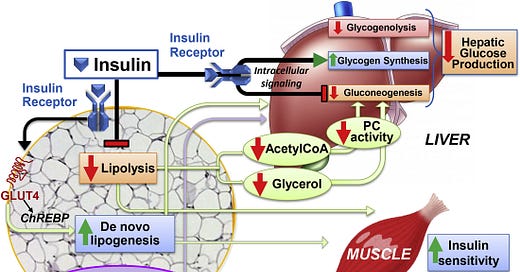
Many clinicians think fat cells are indolent, just sitting there and making no metabolic contribution. Nothing could be farther from the truth. Insulin stimulates glucose uptake in multiple cells especially myocytes and adipocytes by increasing the surface glucose receptor, Glut 4. But what muscle and fat cells do with glucose is different. Muscle in the largest depository for glucose and stores glucose as glycogen and ultimately uses it for energy. Fat cells synthesize glucose into free fatty acids (FFAs) which are stored as fat. This fat is broken down (“lipolysis”) and the FFAs are released during periods of low insulin levels such as overnight or when fasting. Insulin not only promotes lipid synthesis in the fat cell but also inhibits lipolysis, thereby preventing the mobilization of FFAs into the circulation.
Figure from (1).Key points from this complex slide are that insulin both decreases lipolysis and increases lipogenesis in fat cells.
Adipocytes are “exquisitely sensitive to insulin” (1) so even small increases in insulin accelerate glucose uptake and FFA synthesis and reduce lipolysis. So small decreases in insulin (or small increases in insulin resistance) increase lipolysis and the release of FFA into the circulation. FFA are taken up by the liver in proportion to their availability meaning that hepatic uptake of FFAs increases when their concentration increases in the blood. The liver does not catabolize a lot of FFAs so FFAs in the liver are either stored leading to fatty liver or synthesizes into triglycerides and shipped into the blood stream as very low density lipoproteins or VLDL. VLDL are very low dense because they contain mostly triglycerides, which are just fat, and fat floats. Consequently, if insulin levels are low as in diabetes, or if the patient and his/her fat cells are insulin resistant, more FFAs enter the blood stream and force the liver to make triglycerides.
The above chart is from a patient I was referred several years ago for management of hypertriglyceridemia. When he presented his glucose and hemoglobin a1c were normal, but over time his a1c increased. This is not the best example, but someone I saw just last week so his data were available. And I have seen this pattern multiple times: high TGs and normal glucose metabolism with diabetes appearing later. These repetitive observations prompted the rule that “Every patient with hypertriglyceridemia is a diabetic want to be”. There are other causes of high TGs, but early insulin resistance should always be considered. I think high TGs appears before high glucose levels because the effect of insulin on muscle and fat cells are different. Myocytes store and then catabolize glucose. Adipocytes use glucose to make fat and adipocytes both store fat and release FFAs into the circulation. I speculate that the “exquisite sensitivity” of fat cells to insulin is responsible for the high TGs appearing before hyperglycemia. Muscle is the key glucose depository, and at early levels of insulin resistance, the muscle’s glucose uptake is not yet impaired.
I caution you in that I have not seen this hypothesis documented in the literature. That could be because it’s not true or because I haven’t searched enough literature. So, I simply ask that you think about the possibility that you are seeing a “diabetic want 2 B” when you see patients with high TGs. See what your experience is over your career and decide whether this is right or wrong. It was certainly not taught to me by anyone.
The clinical import? Consider an oral glucose tolerance test in patients with high TG’s even if the a1c is not low. It doesn’t have to be high, just not low. If there is evidence of oral glucose intolerance recommend weight loss, exercise and medications since these interventions delay the onset of frank diabetes in individuals with abnormal oral glucose tolerance.
1. Santoro A, McGraw TE, Kahn BB. Insulin action in adipocytes, adipose remodeling, and systemic effects. Cell Metab. 2021 Apr 6;33(4):748-757. PMID: 33826917






From my Pediatric Endocrinologist wife:
This is exactly what I observed in practice- especially in my slew of obese PCOS patients.
Dr. This is happened to me. I believe these meds help increase my A1c to 5.9. And Gl to 105 110. I am trying Metformin for 3 months. Chris.