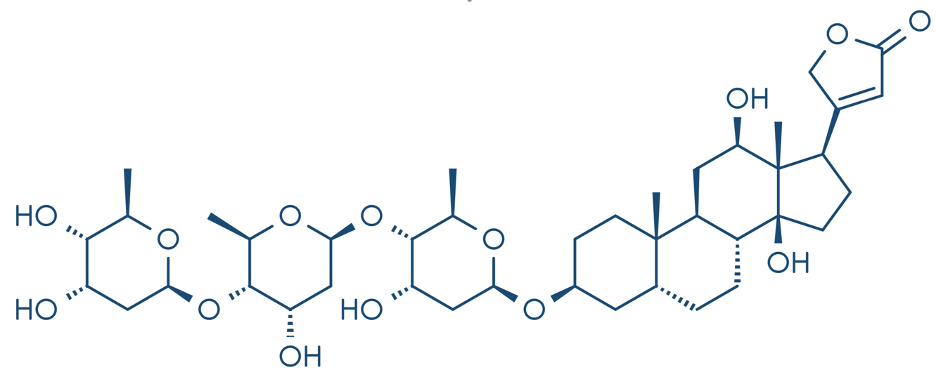
The digoxin molecule reproduced from Shutterstock by Subscription
(Note that the right side of the molecule looks a lot like estrogen, which we’ll discuss later in the post.)
So, let’s finish up the 239-year digoxin story and discuss what you need to know to use digoxin effectively.
1. Digoxin works great at controlling the resting ventricular response in patients in afib and aflutter, especially when there are contraindications to beta blockage or when beta blockage alone is not sufficient. Digoxin can be used long-term, but I usually use it only until I can use other drugs, cardiovert the patient or have the rhythm ablated.
2. Like many anti-arrhythmic, digoxin doesn’t work at all until the patient is fully loaded with the drug. Please read that again because many clinicians don’t give an adequate loading dose and then think the drug doesn’t work.
3. Digoxin is cleared by the kidney, but renal function does not alter the loading dose. Renal function only alters the maintenance dose. You should probably read that again as well.
4. The loading dose is 0.75 mg over 24 hours in a normal sized person, and 1.0 mg in a large person. (I do not have definitions for “normal” and “large” persons, but to paraphrase Supreme Court Justice Potter Stewart, when he was asked in 1964 to define obscenity, “you’ll know it when you see it.”
5. Please load hospitalized patients intravenously (IV) so that you know that the digoxin got into them and so you can see if it worked.
6. I am usually in a hurry to control the HR so I give 0.25 mg IV at 30 to 60 min intervals for 3 doses to reach the 0.75 mg loading dose.
7. You can give an additional 0.25 mg to a large person if there is an insufficient response, but I usually wait for 8 hours after the last dose. Digoxin has therapeutic peaks at 0.5 and 6 hours so the delay is to see the effect after all the doses before increasing the load to 1 mg.
8. If you get no response to the digoxin, make sure you are treating afib and not multifocal atrial tachycardia (MAT), which does not respond to digoxin. MAT is irregularly, irregular and is often mistaken for afib.
9. If I am going to start digoxin in an outpatient, I give 0.25 mg three times the first day as the loading dose. Without the loading dose, it takes about a week for a patient with normal renal function to be fully loaded.
10. The usual maintenance dose is 0.25 mg in patients with a normal creatinine clearance, but I often use a lower dose, such as 0.125 daily or alternating 0.25 with 0.125 daily in older patients until I can get a digoxin level. There are formulae available for determining the replacement dose in renal dysfunction.
11. I do not measure a digoxin blood level during loading, but I do get one once the patient is on a stable maintenance dose to make sure I am not giving too much digoxin. The digoxin blood level in the Digitalis Investigation Group’s study of digoxin risk/benefit in heart failure (HF) was 0.5 to 2. 1
12. The digoxin level does not tell you if you are giving an effective dose. The heart rate does that. The dig level tells you if the patient is taking the drug, and if the level is over 2, that you are giving too much of the drug. I try to use the lowest does possible to achieve the HR control and to obtain a reasonably low dig level.
13. Remember that digoxin levels can increase with the “mycin” antibiotics and with anti-fungals.
There is one other issue with digoxin that is rarely discussed because I don’t think a lot of people know about it. I mentioned earlier that the digoxin molecule had a steroid-like appearance. In fact, digoxin has estrogenic-properties. The high digoxin doses we used in the early 1970’s to control the afib rate could produce gynecomastia in men and uterine break-through bleeding in women with an intact uterus, just like unopposed estrogen. Some proposed that digoxin might be a selective estrogen receptor modulators (SERM), like raloxifene,2 but an analysis of the Nurses Health Study reported that women who used digoxin for >4 years had a 45% increase in breast cancer.3 Digoxin users were more likely to have had mammograms, however, and to have used postmenopausal estrogen. Nevertheless, a meta-analysis of prior studies in the same report suggested that digoxin increased breast cancer risk 20 to 45%.3 Digoxin lowered the risk of prostate cancer. I really don’t know what to do with these data. But they reaffirm the idea of using digoxin primarily for short-periods of time to manage afib or aflutter or longer term in heart failure patients when symptomatic benefit outweighs these potential risks.
Whew! So, that’s it. Two posts on digoxin. But that’s not a digoxin overdose considering it’s been around for 239 years. Digoxin is having somewhat of a renaissance,4 so you might want to at least consider using it in patients with afib and hard to slow ventricular responses, in aflutter, and in patients with still-symptomatic heart failure. Like Mikey in the 1972 Life Cereal advertisement, “Try It, You Might Like It.”
1. Schussheim DH, Schussheim AE. Is digoxin a designer oestrogen?Lancet. 351(9117):1734. 1998 PMID: 9734913
2. Packer M.N End of the oldest controversy in medicine. Are we ready to conclude the debate on digitalis? Engl J Med. 1997 Feb 20;336(8):575-6. PMID: 9023096.
3. Ahern TP, Tamimi RM, Rosner BA, Hankinson SE. Digoxin use and risk of invasive breast cancer: evidence from the Nurses' Health Study and meta-analysis. Breast Cancer Res Treat. 2014 Apr;144(2):427-35. PMID: 24573543.
4. Kotecha D, Bunting KV, Gill SK, et al. Effect of Digoxin vs Bisoprolol for Heart Rate Control in Atrial Fibrillation on Patient-Reported Quality of Life: The RATE-AF Randomized Clinical Trial. Rate Control Therapy Evaluation in Permanent Atrial Fibrillation (RATE-AF) Team.JAMA. 2020 Dec 22;324(24):2497-2508. PMID: 33351042



thank you -